How Long Does It Take for a Dental Implant to Heal Completely?

How Long Does It Take for a Dental Implant to Heal Completely?
“I’m considering a dental implant, but how long will I be recovering? Will I be in pain for months? When can I eat normally again?”
If you’re facing tooth loss and considering a dental implant, understanding the healing timeline is crucial for planning your treatment and managing expectations. The questions about recovery time are among the most common concerns patients express—and understandably so. Dental implant placement is a surgical procedure, and knowing what to expect during the healing process helps you prepare practically and emotionally.
The healing timeline for dental implants is more complex than simply counting days until you “feel better.” While initial surgical healing occurs relatively quickly, the biological process that makes implants successful—osseointegration, where bone fuses to the titanium implant—takes several months to complete.
However, here’s the encouraging news: You won’t spend months in pain or unable to function normally. Most patients feel recovered from the surgical procedure within days to weeks, can eat comfortably (with some modifications) almost immediately, and resume normal activities quickly. The lengthy “healing time” refers to the biological bone integration happening beneath the surface, not prolonged discomfort or disability.
This comprehensive guide breaks down the complete dental implant healing timeline from surgery through final restoration, explains what happens at each stage, identifies factors affecting healing speed, and provides realistic expectations for each phase of recovery. Whether you’re planning your first implant or trying to understand what to expect during the healing process, this information empowers you to approach treatment confidently and prepare appropriately.
Understanding the Complete Dental Implant Process

Before diving into healing timelines, it’s essential to understand what dental implant treatment involves and why healing occurs in distinct stages.
What Is a Dental Implant?
A dental implant is a titanium post surgically placed into your jawbone to serve as an artificial tooth root. This post eventually supports a crown (the visible tooth portion), creating a replacement tooth that looks, feels, and functions like a natural tooth.
The implant system consists of three components:
- The implant fixture (titanium post embedded in bone)
- The abutment (connector piece attached to the implant)
- The crown (custom-made artificial tooth attached to the abutment)
The entire system works together to replicate natural tooth structure and function.
Why Dental Implants Require Healing Time
Unlike other dental restorations like crowns or bridges that are completed in one or two appointments, dental implants require time for biology to work. The process succeeds because of osseointegration—the biological fusion between titanium and living bone tissue.
When the titanium implant is placed in your jawbone, your body recognizes it as biocompatible rather than foreign. Over several months, bone cells grow directly onto the implant surface, integrating it into your jaw structure. This biological integration is what makes implants so stable and long-lasting.
This process cannot be rushed. Bone growth occurs at a natural biological pace that varies among individuals but generally requires 3-6 months for secure integration.
💡 Quick Tip: Think of osseointegration like a broken bone healing. Just as fractured bones require weeks to months to heal properly regardless of how you feel, dental implants need time for bone to integrate even though you feel fine much sooner.
The Complete Dental Implant Healing Timeline: Stage by Stage
Understanding the complete timeline from surgery through final restoration helps you plan realistically and know what to expect at each phase.
| Timeline | Stage | What’s Happening | What You Experience |
|---|---|---|---|
| Day 0 | Implant Placement Surgery | Titanium implant surgically placed into jawbone | Local anesthesia; minimal discomfort during procedure |
| Days 1-3 | Immediate Post-Surgical Phase | Blood clot formation; initial tissue healing begins | Peak swelling and discomfort; managed with medications |
| Days 4-14 | Early Healing | Soft tissue healing around implant; inflammation subsides | Decreasing swelling; improving comfort; dietary modifications |
| Weeks 2-8 | Soft Tissue Healing Complete | Gums healed over implant; surface recovery complete | Normal appearance and comfort; feel “recovered” |
| Months 2-4 | Osseointegration Phase (Lower Jaw) | Bone cells growing onto implant surface; biological fusion | No symptoms; implant buried beneath healed tissue |
| Months 2-6 | Osseointegration Phase (Upper Jaw) | Continued bone integration in upper jaw (takes longer) | No symptoms; life proceeds normally |
| Month 3-6 | Abutment Placement (if two-stage) | Minor procedure to expose implant and attach abutment | Brief appointment; minimal discomfort; heals in days |
| Month 3-6 | Final Crown Placement | Custom crown attached to implant | Complete! Full function restored |
Total Timeline: 3-6 months from implant placement to final crown
Feeling “Normal”: 1-2 weeks after surgery
Full Function: After final crown placement
Stage 1: Immediate Post-Surgery (Days 0-3)
The first 72 hours after implant placement represent the most crucial period for proper healing. Understanding what happens during these initial days helps you prepare and manage this phase successfully.
What’s happening in your mouth:
- Blood clot forms around the implant site, protecting the surgical area
- Initial inflammatory response begins—a normal part of healing
- Soft tissue starts the healing process
- Bone begins the complex biological changes leading to osseointegration
What you’ll experience:
Discomfort level: Moderate, well-managed with prescribed pain medication. Most patients describe the sensation as pressure or soreness rather than sharp pain.
Swelling: Peaks around day 2-3, then gradually subsides. Ice packs during the first 24-48 hours minimize swelling effectively.
Bleeding: Minor oozing for 12-24 hours is normal. Biting on gauze pads controls bleeding easily.
Diet: Soft, cool foods only. Examples include yogurt, smoothies, mashed potatoes, pudding, and ice cream.
Activities: Rest recommended. Avoid strenuous exercise, bending over, or activities increasing blood pressure to your head.
💡 Quick Tip: Set alarms for taking pain medication on schedule during the first few days rather than waiting until you’re uncomfortable. Preventing pain is easier than treating it after it develops.
Most patients report that the first 2-3 days require rest and pain management, but discomfort is manageable with medications. By day 3, most people notice significant improvement.
Stage 2: Early Healing (Days 4-14)
The first two weeks mark rapid improvement in how you feel, though complete healing continues beneath the surface.
What’s happening:
Soft tissue healing progresses rapidly during this period. The gum tissue around your implant closes over the surgical site (in two-stage procedures) or adapts around the healing abutment (in one-stage procedures).
Inflammation decreases substantially. The normal post-surgical swelling and tenderness diminish progressively each day.
Bone begins remodeling around the implant. While you can’t feel this happening, the biological process of osseointegration is initiating at the cellular level.
What you’ll experience:
Pain: Significantly reduced or gone entirely by day 7-10. Most patients discontinue pain medication within the first week.
Swelling: Noticeably decreased. Any remaining swelling is usually minimal by day 7.
Eating: Gradual progression to more normal diet. Soft foods that don’t require aggressive chewing become comfortable. Many patients eat most normal foods by week 2, just avoiding the implant area and very hard items.
Appearance: Surgical site looks increasingly normal. Any bruising fades, redness decreases, and the area blends with surrounding tissue.
Activities: Can resume most normal activities including work, light exercise, and social activities. Avoid contact sports or activities risking trauma to the surgical area.
Many patients feel completely “back to normal” by the end of week 2, though they’re instructed to continue avoiding very hard or crunchy foods at the implant site.
🔑 Key Takeaway: The most challenging part of dental implant recovery is the first week. By week 2, most patients feel recovered and resume normal life, even though biological healing continues for months beneath the surface.
Stage 3: Soft Tissue Healing Complete (Weeks 2-8)
After the initial 2-week period, your soft tissue healing is essentially complete. The gums look and feel normal, and from an external perspective, you appear fully healed.
What’s happening beneath the surface:
Osseointegration accelerates. While you feel fine, the critical bone-to-implant fusion is progressing actively. Bone cells migrate onto the titanium surface, gradually creating stronger biological bonds.
Bone remodeling occurs as your body adapts to the implant presence. Old bone tissue is resorbed and new bone forms around the implant in a pattern that will eventually make it as stable as a natural tooth root.
What you’ll experience:
Zero symptoms for most patients. You won’t feel the osseointegration happening—there’s no discomfort associated with bone integration.
Normal eating with reasonable precautions. Avoid using the implant area for chewing very hard foods, but otherwise eat normally.
No visible changes to the surgical area. It looks healed and blends completely with surrounding tissue.
Normal oral hygiene can resume. Brush and floss normally, being gentle around the implant site initially then treating it like your other teeth.
Life proceeds normally. Work, exercise, social activities—all return to regular patterns.
From your perspective, you’re healed. The fact that bone integration continues for several more months is invisible and asymptomatic.
For comprehensive dental implant treatment in Gandhinagar using advanced techniques that promote optimal healing, patients throughout the region trust experienced implant specialists who guide them through each recovery stage.
Stage 4: Osseointegration Phase (Months 2-6)
This is the longest phase of healing, yet paradoxically the phase during which you experience the fewest symptoms. Understanding osseointegration helps you appreciate why this time is necessary despite feeling completely fine.
What osseointegration means:
Osseointegration is the biological fusion between living bone tissue and the titanium implant surface. At the microscopic level, bone cells called osteoblasts deposit new bone matrix directly onto the titanium, creating a structural and functional connection.
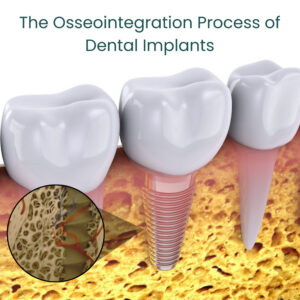
This process transforms the implant from a surgically placed foreign object into an integrated part of your jaw structure, capable of withstanding the forces of chewing—up to 200 pounds of pressure on back teeth.
Timeline differences:
Lower jaw (mandible): 3-4 months for adequate osseointegration
Upper jaw (maxilla): 4-6 months for adequate osseointegration
Why the difference? Lower jaw bone is denser and more compact, allowing faster integration. Upper jaw bone is more porous and has lower density, requiring additional time for secure fusion.
What determines when integration is complete:
Your implant dentist assesses osseointegration success through several methods:
- Percussion testing: Tapping the implant produces a clear, ringing sound when properly integrated versus a dull sound when movement exists
- Stability testing: Measuring resistance to rotation or movement
- Radiographic evaluation: X-rays showing bone in direct contact with implant surface
- Resonance frequency analysis: Sophisticated electronic testing measuring implant stability
What you experience during osseointegration:
Absolutely nothing. This phase is completely asymptomatic. You won’t feel bone growing onto the implant. There’s no discomfort, no changes to the area, no restrictions beyond avoiding extreme forces at the implant site.
Your daily life is completely normal during these months. The healing happening is biological and invisible.
💡 Quick Tip: Think of osseointegration like a tree growing roots. You can’t see or feel it happening daily, but over months, the root system becomes incredibly strong. Your implant is developing its “roots” in your jawbone during this period.
Stage 5: Abutment Placement (Two-Stage Procedures)
Not all patients require this stage—it depends on whether your surgeon used a one-stage or two-stage implant protocol.
Two-stage approach: Implant is placed and covered completely by gum tissue. After osseointegration, a minor second surgery exposes the implant and attaches the abutment (connector piece).
One-stage approach: Implant is placed with healing abutment protruding through gums from the beginning, eliminating need for second surgery.
If you need abutment placement surgery:
The procedure is much simpler than the original implant surgery. Your dentist makes a small incision in the gum tissue over the healed implant, attaches the abutment to the implant, and closes the tissue around it.
Recovery is minimal—usually just a few days of minor tenderness. Most patients manage with over-the-counter pain relievers or don’t need medication at all.
Healing before crown placement takes 1-2 weeks, allowing gum tissue to adapt around the abutment and create natural contours.
💡 Quick Tip: If your surgeon used a two-stage approach, don’t be discouraged by needing a second procedure. This method is often chosen for situations where it provides better long-term results, and the second surgery is much easier than the first.
Stage 6: Final Crown Placement
 This is the exciting stage—the culmination of months of healing when you finally receive your permanent crown and regain complete function.
This is the exciting stage—the culmination of months of healing when you finally receive your permanent crown and regain complete function.
The process:
Impressions of your implant, surrounding teeth, and bite relationship are taken to create a custom crown matching your natural teeth perfectly.
Temporary crown might be placed while your permanent crown is fabricated, allowing you to have something to chew with during the 1-2 weeks required for crown creation.
Final crown placement involves removing any temporary, ensuring perfect fit of the permanent crown, and securing it to the abutment. This appointment is completely comfortable—no anesthesia typically needed.
What you’ll experience:
Immediate function. Once your crown is placed, you can use it for eating immediately (though starting with softer foods and gradually progressing to harder items is recommended).
Natural feel. Modern crowns are shaped and contoured to feel like your natural teeth. Within days, you won’t consciously notice the implant crown as different from your natural teeth.
Complete aesthetic integration. Custom-shaded crowns match your adjacent teeth, making the implant virtually indistinguishable from natural teeth.
This marks completion of your dental implant treatment. While the bone continues remodeling around the implant for months afterward, from a functional and practical standpoint, your treatment is complete.
For patients seeking expert dental care in Gandhinagar throughout all stages of implant treatment, experienced practitioners ensure each phase proceeds optimally toward successful restoration.
🔑 Key Takeaway: The dental implant process unfolds in stages over several months, but you only experience active recovery during the first 1-2 weeks. The remaining healing is biological, asymptomatic, and doesn’t restrict your normal life.
Factors That Affect Your Personal Healing Timeline
While the general timeline provides useful guidance, individual healing varies based on several factors. Understanding what influences your healing speed helps set realistic expectations.
Location of Implant
Upper jaw versus lower jaw significantly affects healing time.
Lower jaw implants typically achieve adequate osseointegration in 3-4 months due to denser, more compact bone structure.
Upper jaw implants generally require 4-6 months because upper jaw bone is more porous and less dense, slowing the integration process.
Posterior (back) versus anterior (front) teeth also matter. Back teeth bear greater chewing forces, so some dentists allow slightly longer healing times to ensure implants can withstand these pressures.
Bone Quality and Quantity
Dense, healthy bone integrates with implants faster and more predictably than compromised bone.
Adequate bone volume allows implants to be placed in optimal positions with good stability. Sufficient bone surrounding the implant on all sides promotes faster, more complete osseointegration.
Poor bone quality or quantity requires additional procedures:
Bone grafting rebuilds inadequate bone before or during implant placement. If grafting is needed, total healing time extends 3-6 months beyond standard implant healing as the graft must integrate before the implant can fully stabilize.
Sinus lift procedures in the upper back jaw create space for implants in areas with insufficient bone height. These add 4-6 months to the treatment timeline.
For patients requiring comprehensive full mouth rehabilitation involving multiple implants and complex bone work, timelines extend accordingly but result in stable, long-lasting restoration.
Overall Health Status
Your general health significantly impacts healing ability:
Good overall health with strong immune function, good circulation, and adequate nutrition promotes faster, more successful healing.
Chronic conditions may slow healing:
Diabetes: Uncontrolled blood sugar impairs healing and increases infection risk. Well-controlled diabetes presents minimal additional risk.
Autoimmune disorders: Conditions affecting immune function may slow healing or affect osseointegration success.
Osteoporosis: Bone-density medications, particularly bisphosphonates, can interfere with bone healing and osseointegration in some cases.
Cardiovascular disease: Compromised circulation may slow healing, though typically not dramatically.
Lifestyle Factors
Smoking is the single most significant modifiable risk factor for implant failure and delayed healing.
Smoking impairs blood flow to healing tissues, reduces oxygen delivery to cells, and interferes with bone formation. Smokers experience:
- Significantly higher implant failure rates
- Slower osseointegration
- More post-operative complications
- Higher infection rates
Quitting smoking before and after implant placement dramatically improves outcomes. Most implant dentists recommend stopping at least 2 weeks before surgery and avoiding smoking for at least 2 months after implant placement.
Nutrition affects healing capacity. Adequate protein intake supports tissue repair and bone formation. Sufficient vitamins (especially C and D) and minerals (calcium, zinc) are crucial for optimal healing.
Oral hygiene practices influence soft tissue healing and long-term implant success. Good hygiene prevents infection that could compromise healing.
💡 Quick Tip: If you smoke, view your dental implant as motivation to quit. The investment you’re making in your implant deserves the best chance of success, and nothing improves those odds more than stopping smoking.
Surgical Technique and Implant Characteristics
Surgeon experience and skill affect both immediate surgical outcomes and long-term success rates. Experienced implant surgeons achieve more predictable osseointegration through optimal implant placement, proper surgical technique, and appropriate case selection.
Implant system quality matters. Modern, high-quality implants with advanced surface treatments promote faster, more complete osseointegration than older or lower-quality alternatives.
Primary stability achieved during surgery—how firmly the implant is anchored in bone immediately after placement—influences healing timeline. Excellent primary stability sometimes allows earlier loading (placing the crown), while poor initial stability requires extended healing time.
What You Can Do to Support Optimal Healing
While biological healing occurs at its own pace, you can influence the process through proper post-operative care and lifestyle choices.
First Two Weeks: Critical Healing Phase
Follow all post-operative instructions precisely:
Medications: Take all prescribed antibiotics completely even when you feel fine. Use pain medication as directed to stay ahead of discomfort.
Ice application: Use ice packs 20 minutes on, 20 minutes off during the first 24-48 hours to minimize swelling.
Rest: Avoid strenuous activity for at least 3-5 days. Elevated blood pressure and increased circulation can worsen bleeding and swelling.
Diet: Stick to soft, cool foods for the first week. Gradually progress to more normal diet as comfort allows, but avoid chewing at the implant site.
Oral hygiene: Don’t brush the surgical site for 24 hours. After that, brush other teeth normally while being very gentle around the implant. Resume gentle brushing of the implant area after one week.
Avoid:
- Smoking or tobacco use
- Drinking through straws (suction can disturb healing)
- Spitting forcefully
- Touching the surgical area with fingers or tongue
- Very hot foods or beverages
- Alcohol consumption
💡 Quick Tip: Prepare soft foods and fill prescriptions before your surgery so everything is ready when you get home. Having someone stay with you for the first 24 hours provides helpful support.
Months 2-6: Osseointegration Phase
Protect the implant site:
While you can eat normally, avoid using the implant for chewing very hard foods like ice, hard candy, or nuts. Excessive force during osseointegration could disrupt the integration process.
Maintain excellent oral hygiene:
Brush twice daily and floss daily around the implant area. Good hygiene prevents gum infection that could compromise osseointegration.
Attend follow-up appointments:
Your dentist monitors healing progress and identifies any concerns early. These check-ups ensure everything is proceeding as expected.
Support your overall health:
Maintain good nutrition, manage chronic health conditions well, avoid smoking, and minimize stress—all factors affecting healing capacity.
Be patient:
Resist the urge to rush the process. Your dentist won’t place the final crown until confident that osseointegration is complete and the implant can handle chewing forces.
For patients seeking experienced dental care near PDPU and Gift City, comprehensive guidance throughout the healing process ensures optimal outcomes and addresses any concerns promptly.
Common Healing Complications and Warning Signs
While most dental implants heal without complications, understanding potential problems helps you recognize issues early when they’re most treatable.
Normal vs. Concerning Symptoms
Normal during first week:
- Mild to moderate discomfort managed with medication
- Swelling peaking around day 2-3
- Minor bleeding or oozing for 12-24 hours
- Bruising visible on gums or face
- Some difficulty chewing
- Numbness that gradually resolves
Concerning symptoms requiring contact with your dentist:
- Severe pain not controlled by prescribed medication
- Swelling that worsens after day 3
- Heavy bleeding that doesn’t respond to pressure
- Fever over 100°F
- Foul taste or odor suggesting infection
- Pus drainage from surgical site
- Implant feeling loose or moving
- Prolonged numbness beyond a few weeks
Infection
Infection signs include increasing pain after initial improvement, swelling that worsens or doesn’t resolve, pus or drainage, fever, and bad taste in your mouth.
If infection develops, contact your dentist immediately. Early treatment with antibiotics and possible site cleaning usually resolves the problem. Untreated infection can compromise osseointegration and lead to implant failure.
Prevention through prescribed antibiotics, excellent oral hygiene, and following all post-operative instructions minimizes infection risk.
Implant Failure
Implant failure is rare—modern implants have success rates exceeding 95%—but can occur.
Early failure (during healing) results from infection, insufficient bone, trauma to the implant, or medical conditions affecting healing.
Late failure (after osseointegration) typically involves peri-implantitis (inflammation around the implant similar to gum disease), overloading from excessive forces, or bone loss from other causes.
Signs of potential failure:
- Implant mobility (it feels loose)
- Pain when chewing
- Gum inflammation around the implant
- Progressive bone loss visible on x-rays
If failure occurs, the implant is removed, the area heals for several months, and a new implant can often be placed successfully after addressing whatever caused the first failure.
💡 Quick Tip: Don’t panic if you experience minor issues during healing. Many small problems resolve with simple treatment. However, never ignore concerning symptoms hoping they’ll improve on their own—early intervention prevents minor issues from becoming major problems.
🔑 Key Takeaway: Most dental implant healing proceeds smoothly without complications. Understanding normal healing patterns versus warning signs helps you recognize the rare occasions when professional attention is needed.
Comparing Healing Times: Dental Implants vs. Other Restorations
Understanding how dental implant healing compares to other tooth replacement options provides perspective on the timeline.
| Restoration Type | Treatment Timeline | Healing Required | Long-term Durability |
|---|---|---|---|
| Dental Implant | 3-6 months total (feel normal in 1-2 weeks) | Osseointegration requires months | 20+ years with proper care; may last lifetime |
| Traditional Bridge | 2-3 weeks (2 appointments) | Minimal; recovery from tooth preparation | 10-15 years average |
| Removable Partial Denture | 3-6 weeks (multiple appointments) | None; immediate use | 5-8 years; requires periodic adjustments |
| Complete Denture | 8-12 weeks after extractions | Gums must heal 6-8 weeks post-extraction | 5-10 years; requires relining/replacement |
Why the implant timeline is worth it:
While dental implants require the longest treatment timeline, they offer advantages other restorations cannot match:
Bone preservation: Implants stimulate jawbone like natural teeth, preventing the bone loss that occurs with bridges and dentures.
Adjacent tooth preservation: Unlike bridges, implants don’t require grinding down healthy adjacent teeth for support.
Superior function: Implants restore nearly 100% of chewing ability versus 50-80% with dentures.
Longevity: Properly maintained implants can last decades or a lifetime, while other restorations need replacement every 5-15 years.
Comfort and convenience: Implants feel and function like natural teeth without the inconvenience of removable appliances.
For patients comparing tooth replacement options in Gandhinagar, understanding both immediate and long-term considerations helps make informed decisions.
Immediate Load Implants: Faster Timeline in Select Cases
For certain patients, immediate load protocols allow placing a temporary crown on the implant the same day as surgery, significantly accelerating the functional timeline.
What Are Immediate Load Implants?
Immediate load (also called immediate function or same-day teeth) involves placing a temporary crown or bridge on dental implants immediately or within 48 hours of implant placement rather than waiting months for osseointegration before loading the implant with a restoration.
This doesn’t speed up osseointegration—bone fusion still requires 3-6 months. However, it allows you to have functional, visible teeth immediately while osseointegration occurs beneath the temporary restoration.
Who Qualifies for Immediate Loading?
Not all patients are candidates. Successful immediate loading requires:
Excellent bone quality and density providing strong primary stability for the implant upon placement.
Adequate bone quantity allowing implant placement in ideal position without grafting.
Good overall health supporting predictable healing.
Specific implant locations: Front teeth (less chewing force) are better candidates than back molars (high chewing forces).
Commitment to dietary restrictions: Immediate load patients must avoid chewing on the temporary crown for months despite its presence.
Advantages and Considerations
Benefits:
- No period without teeth
- Immediate restoration of appearance and basic function
- Fewer total appointments
Considerations:
- Temporary crown must be protected from excessive force
- Not suitable for heavy chewers or teeth grinders
- Higher technical demands on surgeon and dentist
- Requires excellent patient compliance with restrictions
Your implant dentist determines whether immediate loading suits your situation based on clinical evaluation and treatment goals.
The Role of Professional Expertise in Healing Success
Surgical skill, treatment planning, and post-operative care significantly influence both healing timeline and ultimate success.
Why Experience Matters
Proper implant placement in optimal position, angulation, and depth promotes predictable osseointegration. Experienced surgeons achieve primary stability that supports successful healing.
Appropriate case selection means identifying which patients are good candidates and which need additional procedures before implant placement. Not all tooth loss situations are appropriate for immediate implant placement.
Quality materials from reputable implant manufacturers perform more predictably than budget alternatives. Established implant systems have decades of research supporting their success rates.
Comprehensive treatment planning considers bone quality, adjacent teeth, bite forces, aesthetic requirements, and patient health factors. Thoughtful planning prevents complications and optimizes results.
Choosing Your Implant Provider
Seek dentists with:
- Specialized training in implant dentistry beyond general dental education
- Significant experience placing implants (ask how many they perform annually)
- Access to advanced imaging technology for precise planning
- Transparent communication about what to expect during healing
- Clear protocols for managing any complications
For comprehensive dental implant treatment from experienced specialists in Gandhinagar, patients benefit from advanced training, modern technology, and proven surgical protocols that optimize healing and long-term success.
Life After Complete Healing: Caring for Your Dental Implant
Once osseointegration is complete and your final crown is placed, your implant requires ongoing care to ensure decades of successful function.
Daily Home Care
Brush twice daily using a soft-bristled brush and gentle technique. Clean the implant crown just as you would a natural tooth.
Floss daily around the implant. Special floss designed for implants and bridges can make this easier if regular floss proves difficult.
Consider a water flosser as an adjunct to traditional flossing. Water flossers effectively clean around implant crowns and beneath any bridgework.
Use non-abrasive toothpaste to avoid scratching the crown surface where scratches can harbor bacteria.
Professional Maintenance
Regular dental check-ups every 6 months allow your dentist to:
- Examine implant health and surrounding gum tissue
- Take periodic x-rays monitoring bone levels
- Professionally clean the implant and crown
- Identify any issues early when they’re most treatable
Professional cleanings remove plaque and tartar accumulation that home care misses, preventing peri-implantitis (inflammation around implants similar to gum disease).
Protecting Your Investment
Avoid excessive force:
- Don’t chew ice, hard candy, or other extremely hard items
- Don’t use teeth as tools (opening packages, etc.)
- If you grind your teeth, wear a nightguard to protect the implant crown
Maintain overall oral health:
- Address decay or gum disease in other teeth promptly
- Don’t smoke—smoking significantly increases long-term implant failure risk
- Manage health conditions like diabetes that affect oral health
Respond to concerns promptly:
- Any bleeding, swelling, or discomfort around the implant warrants evaluation
- Don’t ignore loose crowns or changes in how the implant feels
With proper care, modern dental implants can last 20+ years and potentially a lifetime. Many implants placed 30-40 years ago in early adopters continue functioning perfectly.
For ongoing comprehensive dental care in Gandhinagar supporting long-term implant success, regular professional maintenance combined with excellent home care preserves your investment for decades.
🔑 Key Takeaway: Complete dental implant healing takes several months, but ongoing care afterward is simple and mirrors care for natural teeth. Your commitment to maintenance determines whether your implant lasts decades or requires replacement.
Making the Timeline Work for You: Practical Planning
Understanding the healing timeline allows you to plan realistically around your dental implant treatment.
Scheduling Considerations
Time off work: Most patients need 1-3 days off for implant surgery depending on their job’s physical demands. Sedentary office work might require only 1-2 days, while physical labor might need 3-5 days.
Special events: If you have important events (wedding, presentation, vacation), plan implant surgery at least 2-3 weeks before or after to ensure you feel your best.
Dental appointments: Budget for 3-5 appointments spread over 3-6 months: consultation, surgery, possible check-ups during healing, abutment placement (if two-stage), and crown placement.
Financial Planning
Total investment for a single dental implant including surgery, abutment, and crown typically represents a significant expense.
Payment timing spreads over months—initial fees at surgery, remaining balance when crown is placed. Some practices offer payment plans making the investment more manageable.
Insurance coverage varies. Some plans cover portions of implant treatment while others don’t. Verify coverage before beginning treatment.
The value proposition: While implants cost more initially than bridges or dentures, their longevity often makes them more economical long-term. A bridge lasting 10-15 years requires replacement, while an implant may last decades without replacement.
Managing Expectations
Be patient with the biological timeline. You cannot rush osseointegration. Attempting to speed the process by loading the implant too early risks failure requiring complete retreatment.
Focus on milestones: Rather than fixating on the months remaining until completion, celebrate each successful phase—surgery recovery, check-up showing good healing, successful abutment placement.
Maintain perspective: The few months of healing provide a lifetime of benefit. Patients who completed treatment years ago never think about the healing timeline—they simply enjoy their functional, stable tooth replacement.
Communicate with your dental team about any concerns or questions during healing. They’re your partners throughout the process and want you to feel informed and confident.
💡 Quick Tip: Consider documenting your implant journey with photos at each stage. Many patients find it motivating to see their progress, and you’ll appreciate having a record of your treatment once it’s complete.
Taking the Next Step: Starting Your Dental Implant Journey
If you’re considering a dental implant but have been hesitant about the healing timeline, understanding what to realistically expect helps you move forward confidently.
Begin with a Consultation
Schedule an evaluation with an experienced implant dentist who can:
- Assess whether you’re a good implant candidate
- Explain your specific treatment timeline based on your situation
- Discuss any bone grafting or other procedures that might be needed
- Answer all your questions about the process and healing
- Provide a detailed treatment plan and cost estimate
Consultations are low-pressure opportunities to learn about your options without committing to treatment.
Questions to Ask
Prepare specific questions:
- What is my expected healing timeline given my specific situation?
- Do I need any bone grafting or other additional procedures?
- What sedation options do you offer for the surgery?
- What will my recovery be like in the first week?
- How many dental implants have you placed?
- What is your implant success rate?
- What if I experience complications during healing?
Understanding your specific timeline based on your clinical situation provides more useful information than general timelines.
Making Your Decision
Consider the complete picture:
- Short-term healing timeline (months)
- Long-term benefit timeline (decades)
- Quality of life improvements from stable tooth replacement
- Bone preservation preventing future problems
- Confidence from natural-looking, functioning teeth
For many patients, the healing timeline seems much more manageable once they understand that “healing” mostly refers to invisible biological processes, not prolonged discomfort or disability.
The few months of healing provide a lifetime of confident smiling, comfortable eating, and stable oral health—a worthwhile investment for most people facing tooth loss.
For comprehensive dental implant consultation and treatment in Gandhinagar near PDPU and Gift City, experienced specialists guide you through realistic expectations, optimal treatment planning, and successful healing toward your permanent tooth replacement.
To learn more or schedule your consultation, visit our Google Business profile to see testimonials from patients who successfully completed implant treatment.
Frequently Asked Questions
How long will I be in pain after dental implant surgery?
Most patients experience moderate discomfort for 2-3 days after implant placement, which is well-managed with prescribed pain medication. By day 4-5, pain typically decreases significantly, and most people discontinue pain medication within the first week. Some minor tenderness may persist for 7-10 days, but it’s usually mild enough that it doesn’t interfere with daily activities. The key to managing post-operative pain is taking medication on schedule for the first few days rather than waiting until you’re uncomfortable—preventing pain is much easier than treating it after it develops. If you experience severe pain that worsens after the first few days or doesn’t respond to medication, contact your dentist as this could indicate a problem requiring attention. Remember that “healing time” and “pain time” are very different—while complete healing takes months, acute pain lasts only days to one week for most patients.
Can I eat normally while my dental implant is healing?
Your diet progresses gradually during implant healing. For the first 3-5 days after surgery, stick to soft, cool foods that require minimal chewing: yogurt, smoothies, mashed potatoes, scrambled eggs, pudding, and ice cream. Avoid very hot foods and beverages as heat can increase bleeding and swelling. By week 2, most patients can eat most normal foods, though continuing to avoid the surgical area for chewing very hard items is wise. During the osseointegration period (months 2-6), you can eat normally with reasonable precautions—avoid using the implant site for chewing extremely hard foods like ice, hard candy, nuts, or tough meats. Once your final crown is placed, you can eat anything you could eat with natural teeth, though starting with softer foods for a few days and gradually progressing to harder items is recommended. Most patients are pleasantly surprised that dietary restrictions are much less limiting than they anticipated, especially after the first week.
What happens if I accidentally put too much pressure on the implant while it’s healing?
Occasional normal forces from accidentally chewing something on the implant side or bumping the area typically don’t cause problems. The concern is about sustained, repetitive heavy forces that could prevent proper osseointegration. If you accidentally bite something hard on the implant side once, don’t panic—monitor the area for unusual pain, swelling, or the implant feeling loose, and contact your dentist if you notice anything concerning. However, intentionally chewing hard foods regularly on the healing implant or subjecting it to trauma through sports impacts or falls could disrupt the integration process. This is why dentists provide specific instructions about avoiding certain activities and foods. If you’re genuinely worried that you damaged the implant through an accident or if the implant feels different after trauma, schedule an evaluation. Your dentist can assess whether the implant remains properly stable. Remember that once osseointegration is complete and your final crown is placed, the implant can withstand normal chewing forces without concern—the restrictions apply mainly during the healing months.
Why does my upper jaw implant take longer to heal than my lower jaw implant?
The difference in healing time between upper and lower jaw implants relates to bone density and structure. Lower jaw (mandibular) bone is significantly denser and more compact, which provides excellent initial stability when implants are placed and allows faster osseointegration—typically 3-4 months. Upper jaw (maxillary) bone is more porous and has lower overall density, especially in the back areas where sinuses create additional challenges. This softer bone requires 4-6 months for adequate osseointegration to achieve the same level of stability that lower jaw bone provides in less time. Additionally, upper back jaw bone may require sinus lift procedures to create adequate space for implants, which adds healing time. The biological process of bone growing onto the titanium implant occurs at different rates depending on bone quality and density. While this means waiting longer for upper jaw implants, the extra time ensures proper integration and long-term success—rushing the process would risk implant failure requiring complete retreatment.
Can I get dental implants if I smoke, and how does smoking affect healing time?
While smokers can receive dental implants, smoking significantly increases failure rates and complications, and most implant dentists strongly encourage quitting before and after surgery. Smoking impairs blood flow to healing tissues, reduces oxygen delivery to bone and gums, interferes with bone formation and osseointegration, increases infection risk, and generally slows healing across all phases. Studies show smokers have 2-3 times higher implant failure rates compared to non-smokers. If you cannot or will not quit smoking permanently, most implant specialists recommend stopping at least 2 weeks before surgery and avoiding smoking for at least 8-12 weeks after implant placement—ideally through the entire osseointegration period. Even this temporary cessation significantly improves outcomes compared to smoking throughout healing. Some dentists refuse to place implants in active smokers due to elevated failure risk, while others proceed with comprehensive informed consent about reduced success probability. If you’re considering implants, view this as powerful motivation to quit smoking—you’re investing significantly in your oral health, and nothing improves your implant’s chances of success more than tobacco cessation. Many patients successfully use implant treatment as the catalyst finally allowing them to quit permanently.










