Why Do I Need a Deep Cleaning If I Already Brush My Teeth Regularly?

Why Do I Need a Deep Cleaning If I Already Brush My Teeth Regularly?
You brush your teeth twice daily, floss regularly, and use mouthwash. Your oral hygiene routine seems thorough, yet your dentist in Gandhinagar recommends a deep cleaning. Your first reaction might be confusion or even frustration: “If I’m already taking such good care of my teeth, why do I need professional scaling treatment?” This is one of the most common questions patients ask, and it reflects a fundamental misunderstanding about what happens beneath the gumline and why even the most diligent home care cannot replace professional deep cleaning.
The answer lies in understanding the difference between regular brushing and professional deep cleaning, how tartar forms in places your toothbrush cannot reach, why gum disease develops despite excellent home hygiene, and what happens during a deep cleaning procedure that makes it medically necessary rather than optional. This distinction is not about questioning your commitment to oral health—it’s about recognizing the limitations of home care and the unique benefits that professional intervention provides.
This comprehensive guide explains why deep cleaning is essential even for people with excellent brushing habits, what signs indicate you need scaling treatment, how gum disease progresses silently below the gumline, and what professional deep cleaning accomplishes that home care cannot. Whether you’ve just received a deep cleaning recommendation or you’re trying to understand why regular cleanings aren’t sufficient, this information empowers you to make informed decisions about your oral health.
Understanding the Difference Between Brushing and Deep Cleaning
Before examining why deep cleaning becomes necessary, it’s crucial to understand what regular brushing accomplishes versus what professional scaling treatment addresses. These are fundamentally different processes targeting different oral health concerns.
Regular brushing removes soft plaque from tooth surfaces above the gumline. Plaque is the sticky bacterial film that constantly forms on teeth throughout the day. When you brush properly twice daily, you disrupt and remove this soft plaque before it hardens into tartar. Brushing also removes food particles, freshens breath, and delivers fluoride to tooth enamel when you use fluoride toothpaste. These benefits are significant and essential for preventing cavities and maintaining overall oral health.
However, brushing has inherent limitations that even the most meticulous technique cannot overcome. Your toothbrush cannot reach beneath the gumline where gum tissue meets tooth roots. This subgingival area—the space between gums and teeth below the visible gumline—is where gum disease begins and progresses. Bacteria colonize these pockets, forming plaque that your toothbrush bristles simply cannot access. Even electric toothbrushes with advanced bristle designs cannot penetrate into gum pockets to remove subgingival plaque.
Deep cleaning, professionally called scaling and root planing, specifically targets the areas your toothbrush cannot reach. Dental professionals use specialized instruments to remove tartar deposits from below the gumline, clean tooth root surfaces where bacteria accumulate, and smooth root surfaces to prevent future bacterial colonization. This process addresses infection and inflammation occurring in gum pockets—problems that develop regardless of how well you brush visible tooth surfaces.
The depth component is literal. Healthy gums attach to teeth with pockets measuring one to three millimeters deep. When gum disease develops, these pockets deepen to four millimeters, five millimeters, or more. Your toothbrush cannot reach four millimeters below the gumline. Professional instruments can, making deep cleaning the only way to remove bacteria and tartar from these disease-causing pockets.
Think of the difference this way: brushing maintains the visible surfaces and prevents new problems from starting, while deep cleaning addresses existing problems that have already developed beneath the surface despite your brushing efforts. Both are essential, but they serve different purposes in oral health maintenance.
How Tartar Forms Despite Regular Brushing
Understanding tartar formation clarifies why even diligent brushers need professional removal. Tartar, also called calculus, is hardened plaque that cannot be removed by brushing or flossing once it forms.
Plaque begins forming on teeth within hours after brushing. This bacterial film develops continuously throughout the day as bacteria in your mouth multiply and create sticky substances that help them adhere to tooth surfaces. Regular brushing removes this soft plaque effectively, which is why twice-daily brushing is recommended—it prevents plaque from accumulating long enough to cause problems.
However, plaque that remains on teeth for approximately 24 to 48 hours begins hardening into tartar through a mineralization process. Minerals from saliva—primarily calcium and phosphate—deposit into the plaque, transforming the soft bacterial film into hard, crusty deposits firmly bonded to tooth enamel. Once this mineralization occurs, the deposits become too hard to remove with brushing. Only professional scaling instruments can break the bond between tartar and tooth surface.
Even people who brush thoroughly twice daily inevitably have small areas where plaque persists long enough to mineralize. These areas include the backs of lower front teeth where saliva glands deposit mineral-rich saliva, the spaces between teeth where bristles don’t reach effectively despite flossing efforts, the gumline where gum tissue meets teeth creating tiny spaces bristles cannot access, and the chewing surfaces of back molars where deep grooves trap plaque.
Certain factors accelerate tartar formation, making some people more prone to buildup despite excellent brushing. Dry mouth conditions reduce saliva flow, which normally helps wash away bacteria and buffer acids. Medications causing dry mouth—including many common drugs for blood pressure, depression, and allergies—increase tartar formation. Smoking alters saliva composition and oral bacteria, promoting faster tartar buildup. Genetic factors affect saliva composition and mineral content, making some individuals naturally prone to heavy tartar formation regardless of hygiene habits.
The location of tartar formation explains why it develops despite brushing. Much tartar accumulates in areas your toothbrush reaches poorly or not at all: between teeth, along the gumline, and especially below the gumline in gum pockets. Subgingival tartar—the deposits below the gumline—causes the most significant problems because it harbors bacteria directly against gum tissue and tooth roots, causing inflammation and infection that progress to gum disease.
For professional removal of tartar buildup and comprehensive gum disease treatment, patients throughout Gandhinagar rely on experienced dental care that addresses both visible and hidden deposits.
Why Gum Disease Develops Below the Gumline
Gum disease begins and progresses in areas your toothbrush cannot reach, which explains why excellent brushing habits don’t prevent it entirely. Understanding this process clarifies why deep cleaning becomes medically necessary.
Healthy gums fit snugly around teeth with shallow pockets measuring one to three millimeters deep—too shallow for significant bacterial colonization. When plaque accumulates along and below the gumline, bacteria in the plaque release toxins that trigger gum inflammation. This initial inflammation, called gingivitis, causes gums to swell and pull slightly away from teeth, creating deeper pockets.
These deeper pockets create a problematic cycle. The increased pocket depth allows more plaque and bacteria to accumulate in spaces even further from your toothbrush’s reach. The bacteria in these pockets multiply in an oxygen-poor environment, where certain aggressive bacterial species thrive. These anaerobic bacteria produce toxins particularly damaging to gum tissue and underlying bone. The body’s immune response to this bacterial presence causes chronic inflammation that, over time, destroys the fibers connecting gums to teeth and the bone supporting tooth roots.
This progression from gingivitis to periodontitis—advanced gum disease—occurs gradually and often painlessly. Most people don’t realize their gum pockets are deepening and bone is being lost because early and moderate gum disease causes minimal symptoms. Gums might bleed occasionally during brushing, or you might notice mild bad breath, but severe pain typically doesn’t occur until disease is advanced.
The insidious nature of subgingival disease explains why regular dental examinations including pocket depth measurements are essential. Dentists use periodontal probes to measure pocket depths around each tooth, detecting disease progression before obvious symptoms develop. Pockets measuring four millimeters or deeper indicate active gum disease requiring intervention beyond routine cleaning.
Several factors increase gum disease risk despite good brushing habits. Genetic predisposition affects how aggressively your immune system responds to oral bacteria—some people develop severe gum disease with minimal plaque while others with heavy plaque buildup maintain relatively healthy gums. Smoking dramatically increases gum disease risk and severity by impairing blood flow to gum tissue and suppressing immune responses. Diabetes affects infection-fighting ability and healing, making diabetic patients particularly susceptible to gum disease. Stress, poor nutrition, hormonal changes, and certain medications all influence gum disease susceptibility.
The key point is that gum disease is primarily a subgingival problem—a disease of the hidden areas below the gumline. Your excellent brushing maintains surface cleanliness but cannot address the bacterial infection developing in pockets your bristles cannot reach.
What Happens During Deep Cleaning That Makes It Essential
Deep cleaning, professionally termed scaling and root planing, accomplishes specific therapeutic goals that regular cleaning and home care cannot achieve. Understanding the procedure clarifies why it’s medically necessary treatment rather than optional extra service.
Scaling removes tartar deposits from above and below the gumline. Dental professionals use specialized hand instruments called scalers and curettes, or ultrasonic scaling devices that vibrate at high frequencies to break tartar’s bond with tooth surfaces. The critical component is subgingival scaling—removing deposits from tooth root surfaces below the gumline within gum pockets. This requires accessing pockets four, five, six millimeters deep or more, removing the hardened bacterial deposits causing inflammation and infection.
Root planing smooths tooth root surfaces after tartar removal. Rough root surfaces created by bacterial toxins and tartar accumulation provide ideal surfaces for bacteria to recolonize. Planing creates smooth root surfaces that resist future bacterial attachment and allow gum tissue to reattach to clean tooth roots. This smoothing process is crucial for healing—rough surfaces would quickly accumulate new plaque and tartar, while smooth surfaces promote gum tissue healing and reattachment.
The procedure typically requires local anesthesia because cleaning deep within gum pockets would otherwise cause significant discomfort. Anesthesia allows the dental professional to clean thoroughly below the gumline without causing pain. For extensive gum disease involving multiple areas, deep cleaning might be divided into quadrant appointments, treating one section of the mouth per visit, or performed in one comprehensive session depending on disease severity and patient preference.
After deep cleaning, gum tissue begins healing within days. The removal of bacterial deposits and toxins allows inflammation to resolve. Over the following weeks, gum pockets shrink as tissue heals and reattaches to cleaned tooth roots. Pocket depth measurements taken several weeks after treatment typically show significant reduction—six millimeter pockets often heal to four or even three millimeters, making them maintainable with regular brushing, flossing, and routine professional cleanings.
However, deep cleaning’s benefits extend beyond immediate healing. Removing subgingival bacteria and toxins prevents continued bone loss that would otherwise progress. Gum disease destroys bone supporting tooth roots—the primary reason adults lose teeth. Halting this bone destruction through deep cleaning preserves the foundation supporting your teeth, preventing loosening and tooth loss. Additionally, research increasingly links gum disease to systemic health problems including heart disease, stroke, diabetes complications, and respiratory disease. Reducing oral bacterial load through deep cleaning may reduce systemic inflammation and associated health risks.
For patients in Gandhinagar seeking professional teeth scaling treatment, comprehensive deep cleaning addresses active gum disease and prevents disease progression that brushing alone cannot control.
Signs You Need Deep Cleaning Despite Good Brushing Habits
Certain symptoms and clinical findings indicate that deep cleaning is necessary regardless of how diligently you brush at home. Recognizing these signs helps you understand why your dentist recommends scaling treatment.
Bleeding gums during brushing or flossing signal gum inflammation, often caused by subgingival plaque and tartar. While occasional minor bleeding might result from aggressive brushing, regular bleeding indicates that bacteria below the gumline are causing inflammatory responses. Healthy gums should not bleed from normal brushing and flossing—persistent bleeding means intervention is needed.
Persistent bad breath or bad taste that doesn’t improve despite brushing, flossing, and mouthwash use often indicates bacteria accumulating in deep gum pockets. The anaerobic bacteria thriving below the gumline produce sulfur compounds creating characteristic unpleasant odors. Surface cleaning cannot eliminate these bacteria because they’re protected in gum pockets—only deep cleaning reaches them.
Gum recession—gums pulling away from teeth exposing more tooth surface or even root surfaces—can indicate underlying gum disease. While recession has multiple causes including aggressive brushing, it often results from bone and tissue destruction due to subgingival infection. Receding gums create spaces where bacteria accumulate, worsening the problem.
Visible tartar buildup along the gumline, particularly behind lower front teeth, demonstrates that plaque is mineralizing despite brushing. If tartar is visible above the gumline, significantly more likely exists below the gumline where you cannot see it. Visible tartar justifies professional scaling even if you have no symptoms.
Gum pockets measuring four millimeters or deeper during dental examinations indicate active or past gum disease requiring deep cleaning. Your dentist measures these pockets around each tooth using a periodontal probe. Measurements of four millimeters or more mean bacteria are colonizing areas your toothbrush cannot reach, making professional intervention necessary.
Loose teeth or teeth that have shifted position suggest advanced gum disease with significant bone loss. While these are late-stage signs, they absolutely indicate that deep cleaning and possible additional periodontal therapy are needed urgently to prevent tooth loss.
Gums that appear red, swollen, or tender rather than firm and pink indicate inflammation typically caused by subgingival bacterial presence. Healthy gums are pale pink, firm, and fit snugly around teeth. Any deviation from this appearance warrants professional evaluation.
X-rays showing bone loss around tooth roots definitively indicate gum disease requiring treatment. Bone loss appears on x-rays as areas where bone level has dropped from its normal height near the crown of the tooth. This bone destruction results from chronic inflammation caused by subgingival bacteria—exactly what deep cleaning addresses.
The Limitations of Home Care and Why Professional Intervention Is Necessary
Even the most dedicated home care regimen has inherent limitations that necessitate professional deep cleaning for certain patients. Understanding these limitations explains why “brushing better” isn’t the solution to gum disease.
Physical access limitations prevent home care from reaching diseased areas. Toothbrush bristles, even with excellent technique, cannot penetrate more than one to two millimeters below the gumline. Floss removes plaque from between teeth but also cannot reach into deep gum pockets. Interdental brushes, water flossers, and other home care adjuncts provide additional benefits but still cannot access subgingival areas where gum disease develops.
Tartar removal requires professional instruments and expertise. Once plaque mineralizes into tartar, it bonds to tooth surfaces with strength that home care implements cannot break. Attempting to scrape tartar off with household items risks damaging gums and enamel. Only professional scaling instruments applied with proper technique can remove tartar safely and effectively.
Visual access presents another challenge. You cannot see below your gumline to identify tartar deposits or assess pocket depths. Professional evaluation includes tools and expertise allowing thorough assessment of areas you cannot see or evaluate yourself. Many patients with significant gum disease are surprised by the diagnosis because they cannot see or feel the problem developing beneath their gums.
Skill and knowledge limitations affect even well-intentioned home care. Proper brushing and flossing techniques require instruction and practice. Many people brush with incorrect technique, missing certain areas consistently or brushing too aggressively, causing damage rather than benefit. Dental professionals can assess your technique, provide personalized instruction, and help you identify areas you’re missing.
The biological nature of gum disease makes home care alone insufficient once disease is established. Active infection in gum pockets cannot be resolved simply by better surface cleaning. The bacteria colonizing deep pockets require physical removal of their tartar habitat and smoothing of root surfaces to prevent immediate recolonization. Home care prevents gum disease from starting and maintains health after professional treatment, but it cannot treat active disease involving deep pockets.
Individual risk factors make some patients more susceptible to gum disease despite excellent hygiene. Genetic predisposition, smoking, diabetes, immune system disorders, and medications affecting saliva flow all increase disease risk. These patients need more aggressive professional intervention because their risk factors accelerate disease development beyond what home care can prevent.
This doesn’t minimize home care’s importance—excellent brushing and flossing are crucial for preventing gum disease and maintaining results after deep cleaning. However, recognizing home care’s limitations helps you understand why professional intervention becomes necessary when gum disease develops.
What to Expect During and After Deep Cleaning
Understanding the deep cleaning process helps alleviate anxiety about the procedure and clarifies what outcomes to expect afterward.
Before beginning, your dental professional will likely administer local anesthesia to numb the treatment area. This ensures comfort during the procedure since cleaning deep within gum pockets would otherwise cause discomfort. The anesthesia numbs gums, teeth, and surrounding tissues, allowing thorough cleaning without pain.
The scaling phase involves removing tartar from tooth surfaces above and below the gumline. Dental hygienists or dentists use manual scaling instruments—specialized curettes designed to reach below the gumline—or ultrasonic scalers that use high-frequency vibrations to break tartar off tooth surfaces. The ultrasonic scaler also flushes the area with water, washing away debris and bacteria. For deep pockets, manual instruments allow precise access to root surfaces within the pocket.
Root planing follows scaling, smoothing tooth root surfaces that were roughened by bacterial toxins and tartar deposits. Smooth root surfaces discourage future bacterial colonization and promote gum tissue reattachment. This phase requires skill and thoroughness to ensure root surfaces are adequately smoothed without removing excessive tooth structure.
The procedure duration depends on disease severity and the number of affected areas. Mild cases affecting limited areas might be completed in one appointment lasting 45 to 60 minutes. More extensive disease might require multiple appointments, sometimes dividing treatment into quadrants (sections of the mouth) treated in separate visits. Severe cases might require two-hour appointments or referral to a periodontist—a gum disease specialist—for advanced treatment.
After deep cleaning, you may experience some tenderness or sensitivity for a few days. Gums might feel sore where they were cleaned, and teeth may be temporarily sensitive to hot, cold, or sweet foods and beverages. Over-the-counter pain relievers typically manage any discomfort. Sensitivity usually resolves within a few days as gums heal.
Gum healing begins within days but continues for weeks. Initially, gums may appear red and inflamed from the procedure itself. As healing progresses, gum color returns to healthy pink, swelling reduces, and pockets begin shrinking as tissue reattaches to clean tooth roots. Your dentist will schedule a follow-up appointment several weeks after deep cleaning to measure pocket depths and assess healing.
Most patients see significant improvement—bleeding stops, bad breath resolves, pocket depths decrease, and gums appear healthier. However, deep cleaning requires commitment to excellent home care afterward. Without proper brushing and flossing, plaque will reaccumulate in pockets, and disease will return. Deep cleaning creates clean conditions allowing healing, but maintaining that healing depends on your daily oral hygiene.
Some patients need more frequent maintenance cleanings after deep cleaning—perhaps every three to four months rather than the standard six months—to prevent disease recurrence. This frequency depends on individual disease severity, risk factors, and how well you maintain home care.
Preventing Future Need for Deep Cleaning
After undergoing deep cleaning, most patients want to know how to prevent needing it again. While some individuals with high genetic risk or systemic factors may need periodic deep cleanings, most people can maintain results with proper home care and regular professional cleanings.
Brush twice daily for two full minutes using proper technique. Many people brush for only 30 to 45 seconds, insufficient to clean all tooth surfaces thoroughly. Use a soft-bristled toothbrush or electric toothbrush, and angle bristles at the gumline where plaque accumulates most heavily. Brush gently—aggressive brushing damages gums without cleaning more effectively.
Floss daily between all teeth. Flossing removes plaque from between teeth where toothbrushes cannot reach. Curve floss around each tooth in a C-shape and slide it gently beneath the gumline on both sides of every tooth. If traditional floss proves difficult, try floss holders, interdental brushes, or water flossers—whatever tool you’ll use consistently.
Consider antimicrobial mouthrinse if your dentist recommends it. While mouthrinse doesn’t replace brushing and flossing, antimicrobial rinses can reduce bacterial populations and help control plaque. Prescription-strength rinses are more effective than over-the-counter products for patients with gum disease history.
Maintain regular professional cleanings at intervals your dentist recommends. For most people, this means every six months, but patients with gum disease history might need cleanings every three to four months. These professional cleanings remove tartar that inevitably forms in hard-to-reach areas despite excellent home care, preventing accumulation that would lead to disease recurrence.
Address risk factors affecting gum health. If you smoke, quitting dramatically improves gum disease outcomes and prevents recurrence. If you have diabetes, maintaining good blood sugar control reduces gum disease risk. Discuss medications causing dry mouth with your physician to explore alternatives or ways to mitigate side effects.
Maintain good overall health through proper nutrition, stress management, and adequate sleep. Systemic health affects oral health—a healthy immune system better controls oral bacteria, and good nutrition supports gum tissue healing and maintenance.
Attend all recommended follow-up appointments after deep cleaning. These appointments allow your dentist to monitor healing, measure pocket depths, and detect any areas where disease might be recurring before significant damage occurs.
For ongoing maintenance after deep cleaning and prevention of gum disease recurrence, residents throughout Gandhinagar including areas near PDPU and Gift City trust professional care that combines thorough cleanings with personalized preventive guidance.
The Connection Between Deep Cleaning and Overall Health
Recent research has revealed significant connections between gum disease and systemic health problems, making deep cleaning more than just an oral health issue—it’s a component of overall health maintenance.
Gum disease has been linked to increased cardiovascular disease risk. The chronic inflammation associated with periodontitis may contribute to atherosclerosis—hardening of arteries—and increase risk for heart attack and stroke. While the exact mechanisms are still being researched, the association is strong enough that cardiologists increasingly recognize oral health as a cardiovascular risk factor.
Diabetic patients face a two-way relationship between diabetes and gum disease. Diabetes increases susceptibility to infections including gum disease, while gum disease makes diabetes harder to control by increasing insulin resistance. Treating gum disease through deep cleaning has been shown to improve glycemic control in diabetic patients.
Pregnant women with gum disease face increased risk for preterm birth and low birth weight babies. The inflammatory response to oral bacteria may trigger early labor or affect fetal development. Many obstetricians now recommend dental evaluation and treatment of gum disease during pregnancy.
Respiratory infections may be more common in people with gum disease. Bacteria from the mouth can be aspirated into lungs, potentially causing pneumonia or worsening chronic respiratory conditions. This is particularly concerning for elderly patients and those with compromised immune systems.
Rheumatoid arthritis shows interesting connections to gum disease, with some research suggesting that oral bacteria may play a role in triggering or worsening this autoimmune condition. Patients with rheumatoid arthritis have higher rates of gum disease, and treating gum disease may help reduce arthritis symptoms.
These systemic connections mean that deep cleaning when needed isn’t just about saving teeth—it’s about reducing whole-body inflammation and potentially lowering risks for serious health conditions. Your dentist’s recommendation for deep cleaning takes into account not just your oral health but your overall wellbeing.
Common Questions and Concerns About Deep Cleaning
Patients often have similar questions and concerns when deep cleaning is recommended. Addressing these helps you feel more comfortable proceeding with necessary treatment.
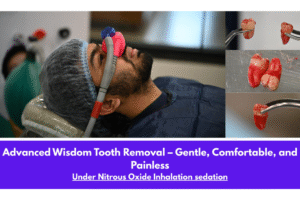
“Will deep cleaning hurt?” With proper anesthesia, deep cleaning should not be painful during the procedure. You might feel pressure or vibration from instruments, but you should not experience pain. After anesthesia wears off, some tenderness is normal for a few days but manageable with over-the-counter pain relievers. If you have dental anxiety, discuss sedation options with your dentist—many practices offer nitrous oxide or oral sedation for anxious patients.
“Why didn’t my previous dentist recommend this?” Different dentists have varying thresholds for recommending deep cleaning, and gum disease progresses over time. You might not have needed deep cleaning at your last visit, but pocket depths and bone loss may have worsened since then. Additionally, some dentists take a more conservative approach, waiting until disease is more advanced before recommending treatment, while others intervene earlier to prevent progression.
“Can’t I just brush better instead?” As discussed throughout this article, brushing cannot reach subgingival areas where gum disease occurs. Improving home care is essential for maintaining results after deep cleaning, but it cannot treat active disease involving deep pockets and tartar buildup below the gumline.
“Is this just an expensive recommendation to make money?” Deep cleaning is a medically necessary procedure for treating gum disease, not an elective cosmetic service. Dentists diagnose need based on clinical findings including pocket depths, bleeding, bone loss visible on x-rays, and tartar presence. Questioning necessity is appropriate, and seeking a second opinion is your right, but recognize that the recommendation is based on objective clinical evidence.
“How long do results last?” With proper home care and regular maintenance cleanings, deep cleaning results often last many years. However, patients with genetic predisposition to gum disease, smokers, diabetics, and others with risk factors may see disease recurrence despite good care. These patients often need more frequent professional cleanings to maintain gum health.
“What happens if I don’t get deep cleaning?” Untreated gum disease progressively worsens, causing continued bone loss, increasing pocket depths, eventual tooth loosening, and ultimately tooth loss. Additionally, chronic oral infection and inflammation may contribute to systemic health problems. While progression varies by individual, gum disease does not improve on its own—without treatment, it invariably worsens.
Making the Decision: Trust Professional Recommendations
When your dentist recommends deep cleaning, several factors should inform your decision-making process.
First, recognize that the recommendation is based on objective clinical findings—pocket depths measured with a periodontal probe, visible tartar, bleeding on probing, bone loss visible on x-rays, and other measurable parameters. These aren’t subjective judgments but evidence-based assessments of disease presence and severity.
Second, understand that dentists have no incentive to recommend unnecessary treatment. The time and expertise required for deep cleaning are significant, and dentists build their practices on trust and patient satisfaction, not on providing unnecessary services. When deep cleaning is recommended, it’s because clinical evidence indicates it’s necessary.
Third, consider the consequences of delaying treatment. Gum disease is progressive—it worsens over time without intervention. Delaying deep cleaning means allowing continued bone loss and tissue destruction. Earlier treatment is less extensive, less expensive, and more successful than treating advanced disease.
Fourth, if you have concerns about the recommendation, ask questions. Why is deep cleaning needed? What clinical findings indicate disease? What are pocket depth measurements? Can I see the x-rays showing bone loss? What happens if I wait? Ethical dentists welcome these questions and provide thorough explanations.
Fifth, if significant doubt remains, seek a second opinion from another dental professional. However, do so promptly rather than delaying for months during which disease continues progressing. Most second opinions confirm the original recommendation because they’re based on objective findings visible to any qualified dentist.
Finally, recognize that deep cleaning, while more involved than routine cleaning, is a common, safe, effective procedure performed thousands of times daily across dental practices. It’s not experimental or particularly risky—it’s standard care for treating gum disease.
For comprehensive evaluation and treatment of gum disease through professional deep cleaning, patients throughout Gandhinagar can access expert care that combines thorough diagnosis, gentle treatment, and personalized preventive guidance supporting long-term oral health.
Frequently Asked Questions
I brush and floss daily. Why would I still need deep cleaning?
Brushing and flossing clean tooth surfaces above the gumline effectively, but gum disease develops below the gumline in pockets your toothbrush and floss cannot reach. Even with excellent home care, tartar forms in small areas where plaque persists long enough to mineralize—particularly along and below the gumline. Once gum disease creates pockets measuring four millimeters or deeper, bacteria colonize these spaces beyond your home care tools’ reach. Deep cleaning uses professional instruments to access these subgingival areas, remove tartar from root surfaces, and smooth roots to promote gum tissue reattachment. Your excellent home care prevents disease from starting and maintains results after deep cleaning, but it cannot treat active disease involving deep pockets. The need for deep cleaning doesn’t reflect failure of your home care—it reflects the biological reality that certain areas are simply inaccessible to brushing and flossing.
How often will I need deep cleaning once I’ve had it done?
Most patients who undergo deep cleaning and then maintain excellent home care with regular professional cleanings don’t need deep cleaning repeated. The procedure treats active gum disease, and if you brush properly twice daily, floss daily, and attend professional cleanings at recommended intervals (every six months for most people, more frequently for those with disease history), your gums should remain healthy. However, patients with genetic predisposition to aggressive gum disease, smokers, diabetics, and those with certain risk factors might need periodic deep cleanings despite good home care because their risk factors accelerate disease development. Your dentist monitors your gum health at each visit through pocket depth measurements and can identify early signs of disease recurrence, allowing intervention before extensive treatment is needed again. The key to preventing repeated deep cleaning is commitment to home care and professional maintenance cleanings.
Is deep cleaning covered by dental insurance?
Most dental insurance plans cover deep cleaning when it’s medically necessary for treating diagnosed gum disease. Insurance companies recognize scaling and root planing as standard treatment for periodontitis, not as elective or cosmetic procedures. However, coverage details vary by plan—some cover the full cost, others cover a percentage, and coverage may depend on factors like how recently you’ve had the procedure. Your dental office can verify coverage with your insurance company before treatment, providing an estimate of your out-of-pocket costs. If you don’t have insurance, many dental practices offer payment plans making treatment affordable. The cost of deep cleaning is significantly less than the cost of treating advanced gum disease complications like tooth loss requiring implants or bridges, making it a worthwhile investment in long-term oral health.
Can I split deep cleaning into multiple appointments if I’m anxious about it?
Yes, deep cleaning is commonly divided into multiple appointments, particularly for patients with extensive disease or dental anxiety. Many dentists treat the mouth in quadrants—upper right, upper left, lower right, lower left—scheduling separate appointments for each section. This approach allows thorough treatment of each area while keeping appointments shorter and more manageable. Between appointments, you can assess how you tolerated the procedure and discuss any concerns with your dentist. Some practices offer sedation options including nitrous oxide (laughing gas) or oral sedation for anxious patients, making treatment more comfortable whether done in one comprehensive session or multiple appointments. The treatment approach should be tailored to your comfort level and clinical needs. Discuss your anxiety with your dentist—they can recommend the approach that works best for you while ensuring thorough treatment of all affected areas.
What’s the difference between regular cleaning and deep cleaning?
Regular cleaning (prophylaxis) is preventive maintenance for healthy mouths, removing plaque and tartar from tooth surfaces above the gumline. It’s typically performed every six months and doesn’t require anesthesia because it doesn’t involve working deep within gum pockets. Deep cleaning (scaling and root planing) is therapeutic treatment for gum disease, removing tartar from below the gumline within gum pockets, cleaning tooth root surfaces, and smoothing roots to prevent bacterial recolonization. Deep cleaning requires anesthesia because accessing deep pockets would otherwise cause discomfort. Regular cleaning takes 30 to 45 minutes and addresses all teeth in one visit. Deep cleaning takes longer—often two to four hours total—and may be divided into multiple appointments. Regular cleaning prevents gum disease in healthy patients. Deep cleaning treats active gum disease in patients with pocket depths of four millimeters or more, bleeding, bone loss, or other disease indicators. Both are important, but they serve different purposes—prevention versus treatment.